All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the Lymphoma Coalition.
The lym Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lym Hub cannot guarantee the accuracy of translated content. The lym and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lymphoma & CLL content recommended for you
Impact of delayed CAR T-cell infusion on clinical outcomes in R/R LBCL
Below, we summarize a retrospective study published by Jallouk et al.1 in Haematologica on the impact of delay in cell infusion after lymphodepleting chemotherapy administration on clinical outcomes in patients with relapsed/refractory large B-cell lymphoma (LBCL).
Study design1
- This was a retrospective study of patients with relapsed/refractory LBCL treated with standard-of-care axicabtagene ciloleucel (axi-cel).
- Delayed cell infusion was defined as axi-cel infusion occurring 6 days after the initiation of lymphodepleting chemotherapy.
- Key outcomes measured included overall response rate, progression-free survival (PFS), overall survival, cytokine release syndrome (CRS), and immune effector cell-associated neurotoxicity syndrome (ICANS).
Key findings1
- Overall, 240 patients were included:
- 40 patients had a delay in axi-cel infusion, due to active infection (n = 34), need for disease-related procedures (n = 3), and logistical reasons (n = 3)
- According to univariate analysis, patients with delayed cell infusion had lower absolute neutrophil count (p = 0.006), lower platelets (p = 0.004), lower hemoglobin (p < 0.001), and higher C-reactive protein (CRP) (p = 0.001) vs patients with on-time infusion
- According to multivariate analysis, patients with delayed cell infusion had lower absolute neutrophil count (p = 0.025) and higher CRP (p = 0.037) than patients with on-time cell infusion
- Patients with delayed infusion had a lower Day 30 overall response rate and complete response rate vs those with on-time infusion (Figure 1)
Figure 1. ORR and CR in patients with delayed infusion vs on-time infusion*
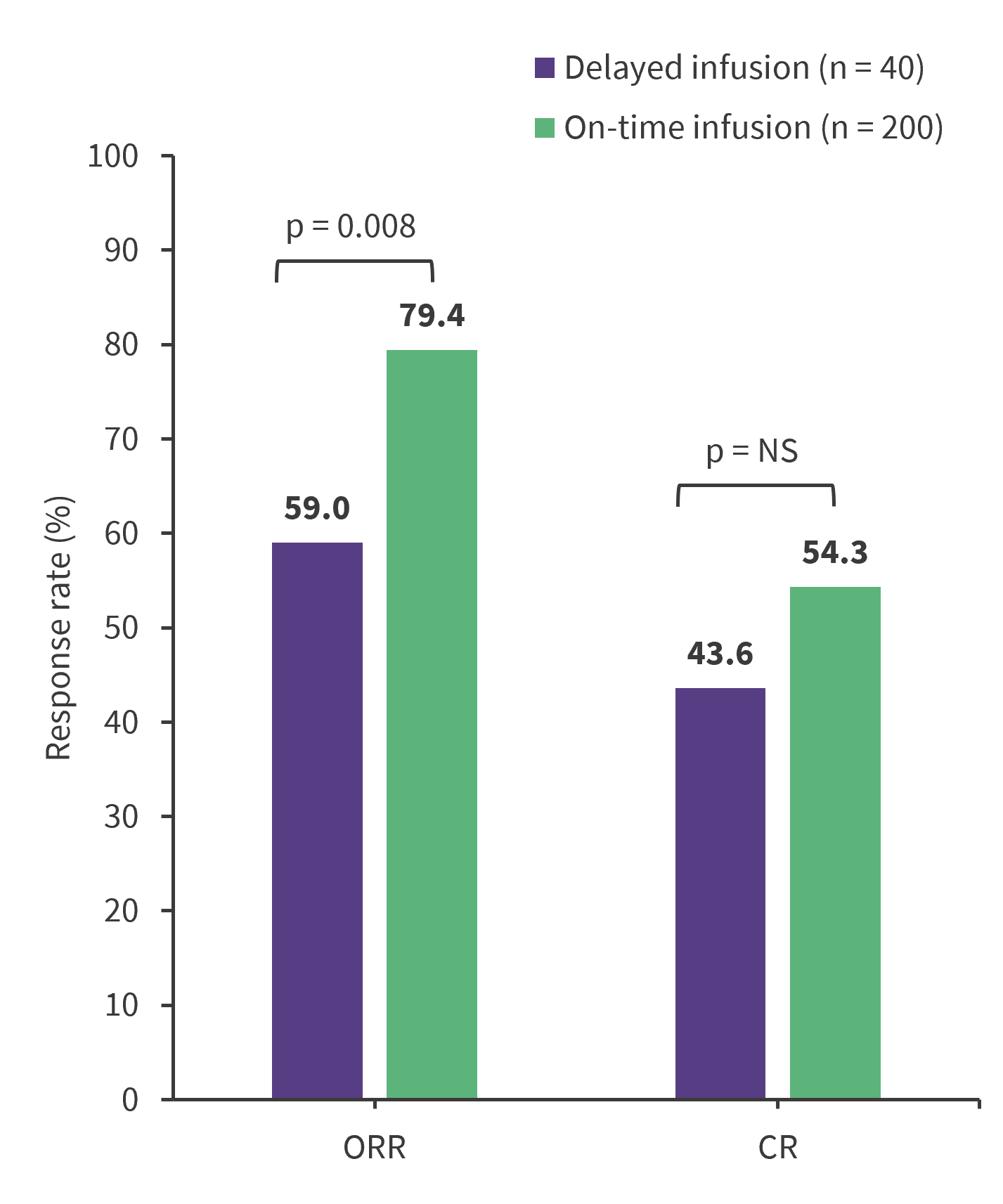
CR, complete response; ORR, overall response rate; NS, not significant.
*Adapted from Jallouk, et al.1
-
- With a median follow-up of 25.7 months, patients with delayed vs on-time infusion had significantly shorter median PFS (3.5 vs 8.2 months; p = 0.002) and overall survival rates (7.8 vs 26.4 months; p = 0.046)
- Patients who experienced delays of 2–5 days and >5 days, but not 1 day, had significantly shorter median PFS (1.8 months and 4.6 months, respectively) than those who had on-time infusion (8.2 months)
- The association between delayed infusion and shorter PFS was maintained on multivariate analysis including age, International Prognostic Index score, lactate dehydrogenase, and CRP
- Patients with delayed cell infusion had similar rates of adverse effects vs those with on-time cell infusion
- Any-grade CRS (90% vs 93.5%) and Grade 3–4 CRS (12.5% vs 8.0%)
- Any-grade ICANS (65% vs 64.5%) and Grade 3–4 ICANS (42.5% vs 39.5%)
| Key learnings |
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

