All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the Lymphoma Coalition.
The lym Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lym Hub cannot guarantee the accuracy of translated content. The lym and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lymphoma & CLL content recommended for you
Development of a novel prognostic scoring system for risk stratification of patients with angioimmunoblastic T-cell lymphoma
Angioimmunoblastic T-cell lymphoma (AITL) represents a subgroup of peripheral T-cell lymphoma arising from the T follicular helper (TFH) cell phenotype and accounting for about 2% of non-Hodgkin lymphomas. The median age at diagnosis is ~ 65 years. Peripheral T-cell lymphoma is characterized by an aggressive course and often presents with advanced-stage disease, B symptoms, elevated lactate dehydrogenase (LDH), and high-risk disease.1
The anthracycline-containing chemotherapy regimen cyclophosphamide, doxorubicin, vincristine, and prednisone is commonly used to treat AITL, with or without the addition of etoposide, and autologous stem cell transplantation (ASCT) may improve outcomes in some patients. However, optimal treatment of AITL remains an unmet need. Therefore, Advani, et al.1 retrospectively analyzed the prognostic impact of clinical covariates and progression of disease within 24 months (POD24) in patients with AITL and developed a novel prognostic score that has the potential to guide new therapeutic approaches.
Study design
Baseline characteristics
A subset analysis of 282 patients with AITL registered in the T-Cell Project (NCT01142674) was performed (Figure 1).
Figure 1. Patients with AITL included in the study*
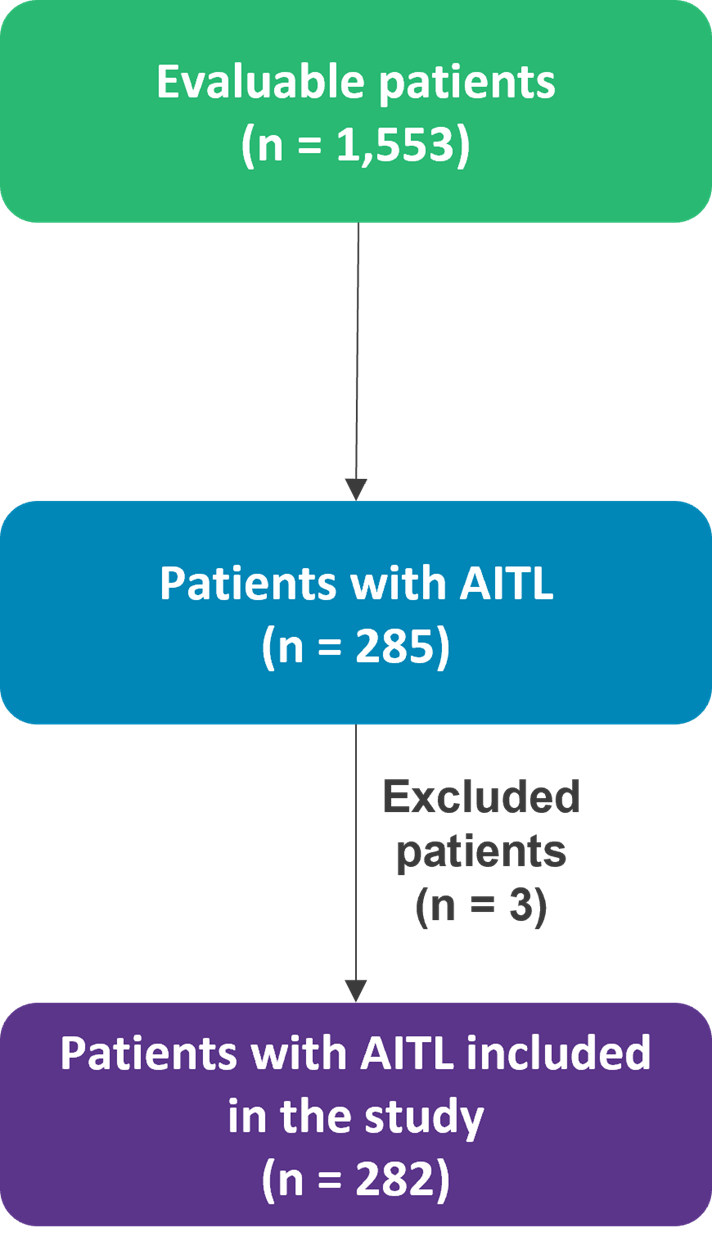
AITL, angioimmunoblastic T-cell lymphoma.
*Data from Advani, et al.1
Eligible patients were adults (age ≥18 years) with AITL, and the median age at diagnosis was 64 years (range, 22–88 years). Of the 282 patients in the AITL subset, 74% had lymphadenopathy, 31% had splenomegaly, 22% had hepatomegaly, 30% had polyclonal hypergammaglobulinemia, and 12% reported hemolytic anemia. Additional demographic characteristics are provided in Table 1.
Table 1. Patient characteristics*
|
ANC, absolute neutrophil count; β2M, β2microglobulin; CRP, C-creative protein; ECOG, Eastern Cooperative Oncology Group; IPI, International Prognostic Index; LDH, lactate dehydrogenase; PIT, prognostic index for T-cell lymphoma; PIAI, prognostic index for angioimmunoblastic T-cell lymphoma; ULN, upper limit of normal. |
|
|
Parameters |
% |
|---|---|
|
Age ≥70, years (n = 282) |
38 |
|
Male, (n = 282) |
60 |
|
Stage III–IV, (n = 282) |
90 |
|
ECOG Performance Status >2, (n = 262) |
31 |
|
B symptoms, (n = 268) |
64 |
|
Bulky disease >5 cm, (n = 282) |
11 |
|
Extra-nodal sites ≥2, (n = 268) |
33 |
|
Bone marrow involvement, (n = 268) |
13 |
|
LDH > ULN, (n = 240) |
58 |
|
Hemoglobin <12g/dl, (n = 261) |
61 |
|
Platelets <150,000/mm3, (n = 262) |
28 |
|
Monocytes <800/mm3, (n = 237) |
76 |
|
ANC > 6500/mm3, (n = 251) |
35 |
|
β2M > ULN, (n = 125) |
79 |
|
CRP > ULN, (n = 151) |
82 |
|
IPI ≥3, (n = 183) |
56 |
|
PIT ≥2, (n = 183) |
62 |
|
PIAI ≥2, (n = 183) |
63 |
Study end points
- The primary end point was overall survival (OS) at 5 years.
- The key secondary end point was progression free survival (PFS) at 5 years.
- A comparison of outcomes between patients with or without POD24 after diagnosis was also made.
- Exploratory end points included comparison of outcomes of patients ≤65 years old in first complete remission (CR1) who did or did not undergo ASCT.
Results
Treatment regimens
Complete treatment data was available for 216 patients and is presented in Table 2. Most patients were treated with anthracycline-based regimens. There was no significant difference in outcomes with or without etoposide.
Table 2. Previous treatment regimens*
|
*Adapted from Advani, et al.1 |
|
|
Treatment regimens (n= 216) |
% |
|---|---|
|
Anthracycline + etoposide |
16 |
|
Anthracycline |
65 |
|
Other chemotherapy regimens |
11 |
|
Supportive care |
8 |
Efficacy
Of the patients who were treated with curative intent (n = 106), 51% achieved complete remission and 18% achieved partial response (PR), with an overall response rate (ORR) of 69%. In total, 13% of patients underwent consolidative ASCT in CR1 and 3% of patients received consolidative radiotherapy. ASCT in CR1 was associated with superior outcomes, including favorable 5-year OS and PFS. Survival outcomes are summarized in Table 3.
Table 3. Survival outcomes*
|
ASCT, autologous stem cell transplant; CR1, first complete remission; CI, confidence interval; OS, overall survival; PFS, progression free survival; POD, progression of disease within 24 months. |
||||
|
Time of data collection |
Patients |
PFS% |
OS% |
p value |
|---|---|---|---|---|
|
At 2 years |
With POD24 (n = 73) |
48 |
63 |
<0.001 |
|
Without POD24 (n = 193) |
2 |
6 |
<0.001 |
|
|
At 3 years |
All patients |
38 (16–43) |
50 (15–64) |
|
|
At 5 years |
All patients |
32 (17–39) |
44 (15–54) |
- |
|
Chemotherapy with Etoposide |
- |
50 (18–68) |
0.769 |
|
|
Chemotherapy without Etoposide |
- |
43 (22–62) |
||
|
Consolidative ASCT in CR1, (n = 27) |
79 |
89 |
0.05 |
|
|
Transplant-eligible patients without ASCT, (n = 56) |
31 |
52 |
0.022 |
|
POD24 was a powerful prognostic factor, with remarkable differences in the PFS and OS of patients with vs without POD24. Of the patients with POD24 (n = 73), 65 died within 24 months, while only 8 were alive at the last follow-up.
Deaths
In total, 128 deaths were recorded, with 48% and 84% of deaths recorded within the first and second year from diagnosis, respectively.
The most common causes of death were
- progressive disease (69%)
- infection (16%)
- second malignancies (1%)
- other treatment-related toxicities (3%)
Prognostic indices
It was observed through multivariate analysis that four variables had the highest prognostic values. This included age ≥60 years, ECOG performance status >2, elevated β2M, and elevated C-creative protein (Table 4). A novel prognostic score, the AITL score, was developed by combining these four covariates to stratify patients into low- (17%), intermediate- (23%), or high-risk (60%) groups.
Table 4. Multivariate analysis for PFS*
|
β2M, β2microglobulin; CI, confidence interval; CRP, C-creative protein; ECOG, Eastern Cooperative Oncology Group; HR, hazard ratio; LDH, lactate dehydrogenase; ULN, upper limit of normal. |
||
|
|
Multivariate analysis |
|
|---|---|---|
|
p value |
HR (95% CI) |
|
|
Age ≥60 years |
0.003 |
2.98 (1.7-6.8) |
|
Extra-nodal sites ≥2 |
0.082 |
3.2 (1.7-5.1) |
|
ECOG performance status >2 |
0.001 |
4.3 (2.1-6.8) |
|
B symptoms |
0.092 |
2.31 (1.8-3.5) |
|
LDH > ULN |
0.071 |
1.73 (1.4-3.1) |
|
Hemoglobin <12g/dl |
0.123 |
0.75 (0.2-2.4) |
|
Monocytes <800/mm3 |
0.082 |
1.31 (0.9-3.3) |
|
β2M > ULN |
0.002 |
3.21 (2.2-6.5) |
|
CRP > ULN |
0.003 |
1.9 (1.2-4.6) |
All prognostic indices identified high-risk subgroups with inferior OS and PFS compared with low-risk patients (Table 5). In comparison with the existing prognostic indices, the AITL score demonstrated the greatest discriminant power with a lower Akaike’s information criterion and higher Harrell C-statistic than the other prognostic indices.
Table 5. Comparison of AITL score with established prognostic indices*
|
AITL, angioimmunoblastic T-cell lymphoma; AIC, Akaike’s information criterion; IPI, International Prognostic Index; NR, not reached; OS, overall survival; PFS, progression free survival, PIT, prognostic index for T-cell lymphoma; PIAI, prognostic index for angioimmunoblastic T-cell lymphoma. |
|||||||||
|
Prognostic index |
IPI |
PIT |
PIAI |
AITL score |
|||||
|---|---|---|---|---|---|---|---|---|---|
|
Risk group (score) |
Low |
High |
Low |
High |
Low |
High |
Low |
Intermediate |
High |
|
Patient, % |
44 |
56 |
38 |
62 |
37 |
63 |
17 |
23 |
60 |
|
Median PFS, months |
34 |
8 |
29 |
9 |
46 |
13 |
31 |
12 |
9 |
|
5-year PFS, % |
40 |
25 |
37 |
27 |
44 |
24 |
41 |
37 |
13 |
|
p value |
0.0006 |
0.03 |
0.006 |
0.003 |
|||||
|
Median OS, months |
NR |
16 |
NR |
17 |
NR |
24 |
NR |
35 |
20 |
|
5-year OS, % |
61 |
32 |
64 |
29 |
61 |
36 |
63 |
54 |
21 |
|
p value |
0.0005 |
0.0002 |
0.001 |
0.0003 |
|||||
|
Harrell C-statistic |
0.697 |
0.648 |
0.711 |
0.785 |
|||||
|
AIC global fit |
566.4 |
575.3 |
543.4 |
524 |
|||||
Conclusion
This study proposed a novel prognostic score—the AITL score—that uses four clinical criteria to classify patients into low-, intermediate-, and high-risk groups with greater discriminant power than established prognostic indices. POD24 was identified as an important prognostic factor for the prediction of OS and use of B2M and CRP were suggested as independent prognostic factors for the prediction of PFS. Major limitations of the study included selection bias and lack of a randomized comparison where higher incidences of bulky disease, elevated LDH, and anemia were observed in the non-transplanted group.
References

